Urinary tract infection (UTI) is a common infection that usually occurs when bacteria enter the opening of the urethra and multiply in the urinary tract. The urinary tract includes the kidneys, the tubes that carry urine from the kidneys to the bladder (ureters), bladder, and the tube that carries urine from the bladder (urethra). The special connection of the ureters at the bladder help prevent urine from backing up into the kidneys, and the flow of urine through the urethra helps to eliminate bacteria. Men, women, and children develop UTIs.
Types
Urinary tract infections usually develop first in the lower urinary tract (urethra, bladder) and, if not treated, progress to the upper urinary tract (ureters, kidneys). Bladder infection (cystitis) is by far the most common UTI. Infection of the urethra is called urethritis. Kidney infection (pyelonephritis) requires urgent treatment and can lead to reduced kidney function and possibly even death in untreated, severe cases.
Signs and Symptoms
Symptoms of lower UTI (e.g., cystitis, urethritis) in adults include the following:
- Back pain
- Blood in the urine (hematuria)
- Cloudy urine
- Inability to urinate despite the urge
- Fever
- Frequent need to urinate
- General discomfort (malaise)
- Painful urination (dysuria)
- Chills
- High fever
- Nausea
- Pain below the ribs
- Vomiting
Complications
Hormonal changes and shifts in the urinary tract during pregnancy increase the risk for kidney infection. Prenatal care includes regular urine testing because bacteria are often present without causing symptoms and UTI during pregnancy may result in complications (e.g., premature birth, high blood pressure) for the mother and fetus. Diseases that suppress the immune system (e.g., HIV) and debilitating diseases (e.g., cancer, sickle cell anemia) increase the risk for UTIs and complications.
Prevention
The following measures can reduce the risk for bladder infections and other UTIs:
- Avoid products that may irritate the urethra (e.g., bubble bath, scented feminine products).
- Cleanse the genital area before sexual intercourse.
- Drink plenty of water to remove bacteria from the urinary tract.
- Do not routinely resist the urge to urinate.
- Take showers instead of baths.
- Urinate after sexual intercourse.
- Women and girls should wipe from front to back after voiding to prevent contaminating the urethra with bacteria from the anal area.
- Avoid constipation.
Treatment
- Antibiotics
- Treatment of underlying source of infection if any
Prostatitis
Prostatitis is an inflammation of the prostate gland. Prostatitis can cause many symptoms, including the following:
- Difficult or painful urination
- Frequent urination
- Fever
- Low-back pain
- Pain in the penis, testicles or perineum (the area between the testicles and the anus)
- Inability to get an erection
- Decreased interest in sex
There are 2 kinds of prostatitis:
- Acute prostatitis
- Chronic prostatitis.
Both are caused by an infection of the prostate. Some kinds of prostatitis may be a result of the muscles of the pelvis or the bladder not working correctly.
Treatment
The treatment is based on the cause : Antibiotics are used to treat prostatitis that is caused by an infection. You might have to take antibiotics for several weeks or a few months. If prostatitis is severe, you might need hospitalisation and treatment with fluids and antibiotics.sometimes prostatitis occurs without infection, it can be hard to treat. Antibiotics are given empirically to treat a hidden infection. Other treatments are aimed at making you feel better.Nonsteroidal anti-inflammatory medicines may help you feel better. Some men get better by taking medicines that help the way the bladder or prostate gland work
Sometimes prostatitis is caused by a sexually transmitted organism, such as chlamydia. However, most cases of prostatitis are caused by infections that are not sexually transmitted. These infections can’t be passed on to sexual partners.
Men who have had prostatitis once are more likely to get it again. Antibiotics may not get into the prostate gland well. Small amounts of bacteria might “hide” in the prostate and not be killed by antibiotics. Once you stop taking the antibiotic, the infection can come again. If this happens, you might have to take antibiotics for a longer period of time to prevent another infection. Prostatitis that is not caused by infection is often chronic. If you have this kind of prostatitis, you might have to take medicine for a long time.Most of the time, surgery is not needed.Although prostatitis can cause you discomfort, it does not cause cancer. If you have prostatitis, your PSA level might go up. This does not mean you have cancer.
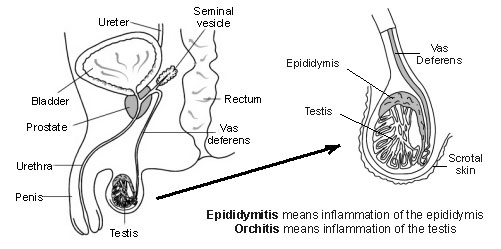
Epididymo-orchitis
- Epididymitis means inflammation of the epididymis.
- Orchitis means inflammation of a testis (testicle).
Most cases of epididymo-orchitis are due to an infection: Bacteria that cause urine infections such as E. coli can sometimes track down the vas deferens to cause an epididymo-orchitis. This can happen at any age and is the most common cause of epididymo-orchitis in men over 35. This is because partial blockage of urine flow becomes more common with increasing age due an enlarged prostate or urethral stricture (narrowing of the urethra). Partial blockage of urine makes you more prone to develop urine infections. A complication of a urine infection is also the usual cause of epididymo-orchitis in young boys.
Sexually transmitted infection
This is the most common cause of epididymo-orchitis in young men (but can occur in any sexually active man). It most commonly occurs with chlamydia and gonorrhoea infections. In men, these infections typically infect the urethra to cause a urethritis. However, sometimes the infection can track down the vas deferens to the epididymis and testis.
Mumps infection in boys also causes epididymo-orchitis in about 1 in 5 cases. The virus gets to the testes via the bloodstream. This cause is now uncommon since the MMR (measles, mumps and rubella) immunisation is now routinely given to children.
An operation to the prostate or urethra
This may allow bacteria into the urethra which may track down to the testes. Epididymo-orchitis used to be a common complication after prostatectomy (removal of the prostate). This is now rare due to better surgical techniques.
Uncommon causes
Infection from other parts of the body can, rarely, travel in the blood to the testes. For example, TB (tuberculosis). Injury to the scrotum can cause inflammation of the epididymis and testis.
Signs & symptoms
Symptoms usually develop quickly – over a day or so. The affected epididymis and testis swell rapidly, and the scrotum becomes enlarged, tender, and red. It can be very painful.
There may be other symptoms if the epididymo-orchitis is a complication from another infection. For example: pain on passing urine if you have a urine infection; a discharge from the penis if you have a urethral infection; etc. As with any infection, you may have a fever and feel generally unwell.
Investigations
A urine test will usually be done if a urine infection appears to be the root cause. A swab of the urethra or other tests may be done if a sexually transmitted infection is thought to be the root cause. Sexual partners of people with epididymo-orchitis caused by a sexually transmitted disease will also need testing.
Tests to look into the urethra and bladder may be needed if a urine infection is the cause, and this is thought to be due to partial blockage of urine flow or other urinary tract abnormalities.
Treatment
A course of antibiotics is usually advised as soon as epididymo-orchitis is diagnosed. These normally work well. Pain usually eases within a few days, but swelling may take a week or so to go down, sometimes longer. The choice of the antibiotic depends on the underlying cause of the infection.
If a sexually transmitted infection is the cause then you should not have sex until treatment and follow up have been completed. Sexual partners of men with epididymo-orchitis caused by a sexually transmitted disease may also need antibiotic treatment.
Antibiotics are not needed if a viral infection is the cause. Supporting underwear and painkillers will ease the pain.
Complications
Most people recover fully and complications are uncommon. Possible complications include:
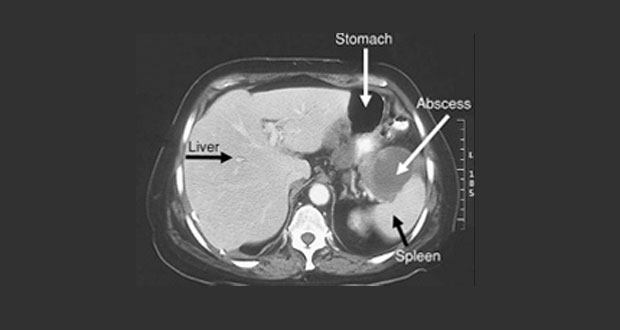
- An abscess (a collection of pus due to infection) occasionally develops in the scrotum. This may need a small operation to drain the pus.
- Reduced fertility in the affected testis, especially in cases caused by the mumps virus.
- An ongoing (chronic) inflammation occasionally develops.Rarely, serious damage to the testis may occur and result in gangrene (dead tissue) in the testis that needs to be surgically removed.
 Urologist in Chennai | Robotic Urologist in India | Chennai Urology
Urologist in Chennai | Robotic Urologist in India | Chennai Urology